Why Does Ozdikenosis Kill You? | Full Explanation of the Fatal Genetic Disorder
Ozdikenosis is a rare, inherited metabolic disease that progressively damages the body at a cellular level. Though only a few hundred cases have been recorded globally, the severity and rapid progression of the disease have drawn the attention of genetic researchers and medical professionals alike.
The question “why does ozdikenosis kill you” is not just rooted in curiosity—it is essential for understanding the mechanisms of this fatal condition and the desperate need for effective treatments.
Ozdikenosis typically appears early in life and is passed down through autosomal recessive inheritance. This means both parents must carry a mutated gene to pass the disease onto their child. The condition deteriorates the body’s organs by disrupting the way cells generate energy, eventually leading to death if left untreated.
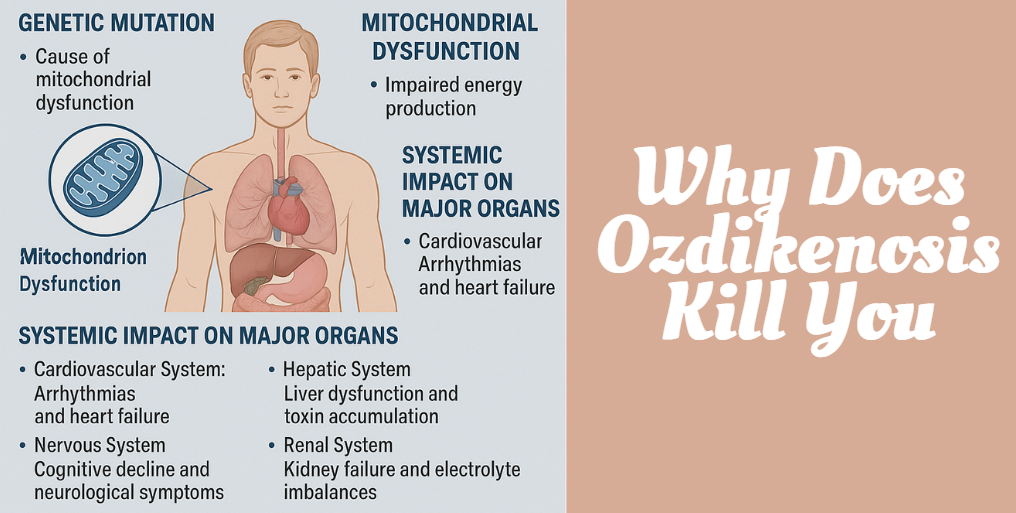
Genetic and Cellular Basis
At its core, ozdikenosis is a genetic condition that affects how the body creates and uses energy. The disease is caused by mutations in specific genes that control mitochondrial function. Mitochondria are tiny, powerful structures in each cell, often referred to as the “powerhouses” because they produce ATP (adenosine triphosphate)—the energy currency of cells.
When these genes mutate, the mitochondria can’t function correctly. This results in:
- Reduced energy production
- Increased oxidative stress (buildup of damaging molecules)
- Cellular damage and premature cell death
The disruption of these cellular processes leads to the failure of organs that require high energy—particularly the heart, brain, liver, lungs, and kidneys.
Mitochondrial Dysfunction: The Core Issue
Understanding why ozdikenosis kills you requires examining mitochondrial dysfunction. Mitochondria generate energy by converting glucose and oxygen into ATP through a process called oxidative phosphorylation. When this process is impaired:
- Energy supply becomes insufficient for vital organs.
- Cells accumulate toxic byproducts.
- Tissues break down due to poor cellular repair and maintenance.
Here’s a simplified table showing how mitochondrial failure affects different systems:
| System Affected | Result of Mitochondrial Dysfunction |
|---|---|
| Nervous System | Neurological decline, memory loss, seizures |
| Cardiovascular System | Weak heart muscles, arrhythmias |
| Respiratory System | Impaired oxygen use, shortness of breath |
| Liver | Toxin buildup, poor detoxification |
| Kidneys | Waste accumulation, electrolyte imbalance |
The cumulative effect is systemic failure, explaining why ozdikenosis progresses so quickly and lethally.
Systemic Impact on Major Organs
Ozdikenosis is not confined to one area of the body—it attacks multiple organs simultaneously. As mitochondria fail, tissues cannot sustain themselves, leading to organ failure.
Cardiovascular Impact
The heart, which demands a high level of energy, begins to falter. Patients may experience irregular heartbeats, thickened heart walls, or congestive heart failure. This can result in sudden cardiac arrest.
Nervous System Deterioration
One of the earliest and most alarming symptoms is the decline in brain function. Children with ozdikenosis may show signs of developmental delay, memory loss, or seizures. As the disease advances, cognitive functions deteriorate completely.
Respiratory Distress
Breathing becomes difficult due to weakened diaphragm muscles and reduced oxygen transport. Pulmonary infections are common and often fatal due to low immunity and energy-starved lungs.
Liver and Kidney Failure
The liver fails to process toxins, while the kidneys can no longer filter blood properly. Both organs play a critical role in balancing the body’s internal environment, and their failure is often the final blow.
Disease Progression Stages
The progression of ozdikenosis is typically rapid. Understanding these stages offers insight into why ozdikenosis kills with such severity:
| Stage | Timeline | Symptoms |
|---|---|---|
| Stage 1 | 0–6 months | Fatigue, developmental delay, poor appetite |
| Stage 2 | 6–12 months | Muscle weakness, vomiting, difficulty breathing |
| Stage 3 | 12–24 months | Neurological decline, seizures, organ stress |
| Stage 4 | 24–36 months | Multiple organ failure, coma, and death |
Without aggressive medical intervention, most patients do not survive past 3 years of age.
Clinical Markers and Diagnostic Tools
Diagnosing ozdikenosis early is critical but challenging due to its rarity. However, several diagnostic tools can help identify it:
- Blood tests: Elevated lactate, low ATP levels, abnormal liver enzymes.
- Genetic testing: Confirms mutations in genes related to mitochondrial function.
- MRI and CT scans: Reveal brain atrophy or damage to other organs.
- Muscle biopsy: Used to examine mitochondrial structure under a microscope.
Diagnosis often happens late, which further reduces the chances of managing the disease effectively.
Treatment and Management
As of now, there is no cure for ozdikenosis. Treatment is primarily supportive, aimed at reducing symptoms and prolonging life.
Supportive Measures Include:
- High-calorie, nutrient-rich diets
- Antioxidant therapy (e.g., Coenzyme Q10)
- Seizure management with antiepileptic drugs
- Mechanical ventilation for respiratory support
- Physical therapy to preserve muscle function
Experimental gene therapies are under investigation, but they are not yet widely available. The lack of a cure plays a large part in why ozdikenosis continues to be a fatal diagnosis.
Prognosis and Survival Rates
The outlook for patients with ozdikenosis remains grim. Most children diagnosed with the condition have a life expectancy of fewer than 36 months. However, early detection and aggressive symptom management can slightly extend life and improve quality.
Factors That Affect Survival:
- Early diagnosis and intervention
- Access to specialized medical care
- Supportive therapies and nutrition
- Family genetic background
Still, even with intervention, the systemic nature of the disease often leads to fatal outcomes.
Living with Ozdikenosis
Living with ozdikenosis is emotionally and physically taxing—for both the patient and caregivers. Daily care includes administering medication, monitoring for seizures or infections, and often, coordinating with a team of specialists.
Support systems, including palliative care, genetic counseling, and social work, are essential in helping families cope. Awareness and advocacy are crucial to funding research for future treatments.
Conclusion
So, why does ozdikenosis kill you? The answer lies in the genetic mutation that cripples mitochondrial function and, consequently, energy production. This disruption cascades through the body, damaging major organs and leading to rapid, fatal decline.
With no known cure and limited treatment options, ozdikenosis remains one of the most devastating metabolic disorders known today. However, through research, awareness, and early intervention, there is hope that the medical community will one day unlock the key to halting this deadly disease.
Recommended Articles
Melekaike Laka: The Hawaiian Christmas Greeting and Its Festive Legacy
Munchabilies THC Trippy: The Ultimate Guide to Psychedelic Cannabis Edibles
Skrawer Wayne Cartoon Book: A Whimsical Journey of Art, Humor & Life Lessons